Recent trends favor use of bracing for knee OA
Experts say new research underscoring the clinical benefits of bracing for patients with knee osteoarthritis (OA), along with more comfortable device designs aimed at improving patient compliance, may help boost the historically low rates of brace utilization in this patient population.

OssKin Evoke
By Barbara Boughton, Lower Extremity Review July 2017
More than 20 million people in the US suffer from knee osteoarthritis (OA), and these numbers are expected to double over the next decade, due to the aging of the baby boomer generation and the obesity epidemic. Ultimately, many patients progress to end-stage OA and require knee arthroplasty.[1] But this may not be the best solution for younger patients, who are likely to outlive at least one implant, if not several. So, increasingly, clinicians are looking at alternative nonsurgical interventions that can help delay the need for knee replacement.
One such option for patients with tibiofemoral knee OA is bracing to offload the affected compartment. Studies indicate that such braces do help to alleviate pain and improve function, and suggest bracing can help patients delay or avoid knee arthroplasty. Research on knee OA bracing has been dogged with limitations, some of which have negatively affected use of the devices in clinical practice, but it appears that tide is starting to turn.
“Bracing is an underused modality, and although use of a brace requires careful patient education and follow-up, clinicians should consider using this treatment method a lot more then they currently do,” said Michael A. Mont, MD, chair of the Department of Orthopaedic Surgery at the Cleveland Clinic in Ohio.
Although many studies on bracing for knee OA have been published in the last 10 years, the results have been conflicting. Most of these studies have also been small and non-randomized, with follow-up times as short as only a few months. In its latest evidence-based guideline on knee OA treatment, published in 2013, the American Academy of Orthopaedic Surgeons (AAOS) concluded the evidence for clinical benefits from braces was “inconclusive.” [2]
“While strong or moderate research evidence shows that anti-inflammatories, weight loss, and exercise help all patients with knee osteoarthritis, we found that braces do not help all patients. Yet, in selected patients, bracing can be a good option,” said Greg Brown, MD, PhD, AAOS section leader for clinical practice guidelines, and physician champion for bundled payments at Catholic Health Initiatives, Franciscan Health, in Tacoma, WA.
Overweight and obese patients as well as those with deformities derive less benefit from braces because it’s more difficult to obtain a good fit on their legs, researchers interviewed by LER said.
| Signs of progress |
Yet, in the last few years, researchers have published randomized clinical trials, longer-term studies, and analytical reviews of clinical trials on tibiofemoral knee OA bracing. New brace designs that provide more comfort and enhanced efficacy have also been highlighted in research—and may help address issues related to poor patient compliance that have long hampered brace use in clinical practice.
Mont has led a number of recently published randomized clinical trials on bracing for knee OA. In a prospective randomized trial published in 2015,[3] Mont and fellow researchers evaluated 26 patients with medial or lateral end-stage knee OA who wore pneumatic unloader braces with an extension assist for three months, and compared outcomes with a matched group of 26 patients who received standard of care.
Functional outcomes in both groups were assessed at three-month follow-up visits with Knee Society Score (KSS) assessments (questionnaires that characterize patient satisfaction, expectations and physical activities) and the Lower Extremity Functional Scale (LEFS), which assesses patient-reported participation in activities of daily living. Patients’ pain was scored using a visual analog scale (VAS) and their physical and mental health were rated with Short Form (SF)-36 surveys. The researchers also evaluated patient performance on tests including Timed Up and Go (TUG), timed stair climb, repeated chair rise, two-minute walk, single-limb step, and isokinetic quadriceps and hamstring muscle strength tests.
Although it has been theorized that braces for knee OA simply offload forces and have no effect on muscle strength, Mont said, he and his research colleagues found brace treatment was associated with a 54% mean improvement in quadriceps strength and a 27% mean gain in hamstrings strength. By contrast, the cohort that received standard care had a mean 8% loss of quadriceps strength and a 1.8% mean loss of hamstrings strength. The patients in the braced group also showed greater improvements in the functional tests than the controls, and the differences were statistically significant for the TUG, stair climbing, and two-minute walking distance tests.
Most importantly, the patients who wore braces experienced significant and dramatic decreases in pain—from a mean of 4.[7] VAS points to 2.8 points—compared with those who received standard care, who had just a slight decrease in pain of .1 VAS points. Patients who wore braces also had significantly greater improvements in the functional scores of the LEFS and the KSS questionnaires.
“In the study, the patients in the brace group had triple the improvements in pain of the standard of care group, even when they were not wearing the brace,” Mont said. “They were also more active. The results showing greater quadriceps and hamstring muscle strength with the brace are important, because improved strength in these muscles provide stabilization for the knee, as well as reducing symptoms.”
| Tabling TKA |
In another long-term study, published in 2016,[4] Mont and colleagues found braces could decrease the need for pain-relieving injections and might delay total knee arthroplasty (TKA). In the study, the researchers analyzed the clinical outcomes of 11 patients who wore a pneumatic unloader brace for severe (Kellgren-Lawrence grade 3 to 4) medial or lateral OA, derived from a longitudinally maintained database of patients from a prospective randomized single-center study. The outcomes at one-year follow-up were compared with those of 25 knee OA patients who received conventional treatment.
A significantly lower percentage of patients in the brace group received pain-relieving intra-articular injections compared with the conventional care cohort (46% vs 83%). The bracing group also was less likely to undergo TKA: At one year, 18% of patients in the braced cohort had undergone TKA, compared with 36% in the unbraced group. The mean time to TKA was also longer in the bracing group than in the conventional care group (482 vs 389 days). However, these differences between groups did not reach statistical significance, due to the small sample size. To further assess the long-term benefits of bracing, the researchers’ goal is to reevaluate the same patients five years from baseline.
The compliance rate in the study was 80%, which is a limitation of the research, Mont and colleagues wrote in the paper. The compliance rate among patients in real life might be lower, given the lifestyle adjustments needed to adequately gain benefits from the brace, the authors noted. Braces can be heavy, some need to be worn outside clothing, and they should be worn at least several hours per day while ambulating—making them inconvenient and even uncomfortable for patients.
“Delaying or avoiding a total knee arthroplasty can be advantageous, since these are substantial surgeries with potential complications and risks,” Mont said. “Braces can also be used to control pain in patients with mild osteoarthritis, helping these patients avoid a knee arthroplasty. Braces should be part of our armamentarium for treating knee OA, since some patients can’t tolerate analgesia and don’t want to undergo six weeks of physical therapy or intra-articular needle injection, which also may not be working.”
| Beyond peak KAM |
In the first meta-analysis of randomized trials of valgus bracing for medial knee OA,[5] published in 2015, Canadian researchers found braces were associated with significant improvements in pain and function.
Yet, several challenges remain for knee OA bracing research, noted lead author Rebecca Moyer, PhD, assistant professor in the School of Physiotherapy at Dalhousie University in Halifax, Nova Scotia, Canada. Studies have yet to define which knee OA patients will benefit the most from bracing, and there is still no definitive research on how braces may alter disease progression. And, assessing peak knee adduction moment (KAM) as a proxy for joint load, as many biomechanical studies have done rather than directly measuring joint load during gait, may also be problematic, she noted.
“Whether that’s truly indicative of a true biomechanical effect is not fully known. We need more studies that look at other measures,” Moyer said.
The good news is that research studies are beginning to look at some of those other measures to assess gait and detrimental forces at the knee and their association with OA and bracing. In a gait study on the effects of decompressive brace use in 15 people with medial knee OA, for instance, Lamberg and colleagues assessed knee adduction impulse, as well as knee adduction moment, knee motion, and walking velocity at baseline and two and eight weeks after patients were fitted with braces.[6]
Knee adduction impulse provides a measure of overall KAM during the entire stance phase—not just the forces at any one point.
“The peak adduction moment does not always correlate to when the patient is having pain,” said lead author Eric Lamberg, PT, associate professor and chair of the Department of Physical Therapy at Stony Brook University in New York. “The cumulative forces going through the knee—not just the forces at one point—are what contribute to pain in knee osteoarthritis patients.”
The results of the gait study indicated knee adduction impulse was reduced by 36% at two weeks and 34% at eight weeks compared with baseline. Participants (who wore the braces an average of six hours a day) also demonstrated a 26% reduction in second peak KAM, and walked faster with increased knee motion during stance compared with baseline.
| Functional benefits |
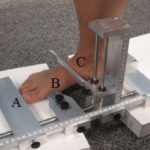
In another longer-term study, published in 2016,[7] Lamberg and colleagues assessed pain, symptoms, and function—including walking abilities, muscle strength, balance, and activities of daily living—after six months of brace wear. Nineteen patients with unilateral medial or lateral compartment knee OA were fitted with a rigid custom brace designed to alter frontal plane alignment and reduce forces on the affected part of the knee.
“The overall goal of bracing is to improve function, and we wanted to see how bracing would affect the outcomes that really matter—patient function, quality of life, and how long patients could walk,” Lamberg said.
Participants were assessed with muscle function tests, a six-minute walk test, and balance tests at baseline and two and eight weeks after brace fitting. In addition, participants filled out the Knee injury and Osteoarthritis Outcomes Score (KOOS) and Activities-specific Balance Confidence (ABC) questionnaires at baseline and two weeks, eight weeks, three months, and six months after brace fitting.
Participants had significant increases in both power and torque during knee extension and flexion at eight weeks, and improved six-minute walk test distances at eight weeks compared with baseline. Scores on the KOOS and ABC surveys were significantly improved compared with baseline.
“Overall, the patients in the study were more active and could walk further, which may have been the reason for the increased muscle strength. The bracing provided stability that had a significant effect on patient activities and quality of life,” Lamberg said.
| Compliance |
Lamberg, like many other knee OA researchers interviewed by LER, acknowledged that compliance can be an issue with knee braces, since they can migrate or cause skin irritation or discomfort, and patients may perceive them as heavy and bulky.
“Braces that provide the most pain relief may also be more rigid and bulkier, so when prescribing a brace, it’s important to provide a brace that will reduce pain and fit the patient’s lifestyle,” he said.
In Lamberg’s 2016 study, patients were seen by orthotists for brace fitting and were instructed in detail about putting on and adjusting the brace. Patients were also followed regularly to assess whether they needed further instruction in brace adjustment. Three patients in the 2016 study had problems with brace slippage, but because of continued follow-up, the patients learned to improve their adjustments and eliminate slippage.
To help reduce complications and improve compliance, Lambert recommends that physical therapists, as well as other clinicians who see these patients regularly, be made aware the patient uses a brace and may need additional education about adjusting it over time.
“In most clinical practices, the typical patient gets a brace from an orthotist and no follow-up,” Lamberg said.
Newer brace designs also are increasing efficacy and reducing the complications that can accompany the use of knee OA braces. In the studies by Mont and colleagues, the researchers used a brace that combined pneumatic joint unloading, active swing-assist, and construction using a flexible and elastically deformable material. The active swing-assist was produced by tensioned elastic bands (based on the patient’s weight) designed to facilitate more rapid knee extension during the late swing phase of gait. The brace design also helped promote the use of the hamstring muscles to control knee extension during the late swing phase, and use of quadriceps muscles during the loading response phase of stance to obtain adequate knee flexion—which explains the improvements in hamstrings and quadriceps strength observed in the study, Mont said.
In a study presented at the French Society of Physical and Rehabilitation meeting in October 2016,[8] researchers led by Etienne Cusin, PhD, of the Université of Savoie Mont Blanc in Chambéry, France, also found that using a dynamic unloader knee brace—which produces a valgus moment only during the stance phase of gait—had the potential to provide biomechanical efficacy without sacrificing comfort.
In the study, researchers quantified knee moments in situ throughout the gait cycle in eight healthy varus patients, and found a dynamic unloader knee brace that was activated during knee extension and inactivated during knee flexion could be helpful.
“Continuous valgus moment exerted by traditional unloader knee braces for osteoarthritis patients can generally be adjusted, and the greater the valgus moment, the higher the decrease in medial knee load,” Cusin said. “Yet, for the highest valgus adjustments, discomfort and poor compliance are frequently reported. Thus, the advantage of a dynamic unloader knee brace is to provide the biomechanical efficacy of the highest valgus adjustment braces solely when necessary [in stance phase], coupled with the typical comfort of neutral valgus adjustment braces.”
Cusin said his research indicates designs of new, innovative braces have the potential to increase patient comfort and compliance.
| Post-traumatic OA |
Along with brace design, research has begun to delve into the question of whether bracing can affect the risk of developing knee OA after anterior cruciate ligament reconstruction (ACLR) and meniscectomy. In one 2016 pilot study of 22 patients who underwent meniscectomy,[9] scientists found peak knee flexion moment increased with bracing during a forward lunge and one-leg rise—which may suggest increased stability of the knee, leading to improved knee function, the researchers wrote.
In another 2016 study,[10] researchers fitted 19 lateral knee OA patients with valgus mal-alignment, who had undergone ACLR five to 20 years earlier, with a varus unloader brace and performed gait analyses. They found the brace, when adjusted for optimal frontal plane alignment, was associated with significantly increased peak knee flexion angle and knee adduction angle and reduced peak knee internal rotation angle compared with no brace. The patients also showed significant increases in peak knee flexion moment, adduction moment, and external rotation moment. With brace wear, the patients also experienced increases in peak hip adduction and decreases in peak hip adduction angle.
“Our study was the first to show that the unloader brace has the potential to alter joint biomechanics in people with knee OA, and it’s plausible that mitigating abnormal biomechanics associated with OA progression may aid in slowing down disease progression after ACL surgery,” said Harvi Hart, PhD, a postdoctoral research fellow in the College of Science, Health and Engineering at La Trobe University in Melbourne, Australia. “But further research is required to determine the long-term effects of bracing on joint biomechanics and progression of OA in ACL-injured patients.”
As Hart noted, this research is preliminary, and the use of braces for preventing knee OA after meniscectomy or ACLR has not yet been widely accepted in clinical practice, according to researchers interviewed by LER. Yet, due to an increasing number of clinical studies that have pointed out benefits of bracing for knee OA, some clinicians are more willing to prescribe them.
| Swaying the skeptics |
Braces should be used as part of a multimodal treatment strategy to treat the symptoms of knee OA and enable increased exercise and activity in these patients, said Roger Ostrander, MD, an orthopedic surgeon and the associate fellowship director for sports medicine and arthroscopy at Andrews Institute in Gulf Breeze, FL.
Ostrander and colleagues published a prospective randomized controlled trial of unloader bracing for medial compartment knee OA in the American Journal of Orthopedics in 2016.[11] In the study, the researchers randomized 31 patients with knee OA to receive an unloader brace or to undergo other conservative treatments. Patients in both groups continued non-steroidal anti-inflammatory and joint supplement use, as well as home exercise, and were assessed four, eight, 16, and 24 weeks after baseline evaluations.
The results indicated the patients in the brace group had significantly less pain, fewer arthritis symptoms, and greater ability to engage in activities of daily living, as assessed by KOOS scores, compared with those who did not receive a brace. VAS scores also showed the brace group had significantly less pain throughout the day compared with those who did not use a brace, and improved activity levels as assessed by weekly patient diaries.
“I was a little surprised by the results, because I wasn’t sure the study would show a benefit for brace use,” Ostrander said. “Before doing the study, I had been skeptical about their use. But, based on our study, I’m now more willing to prescribe bracing. It’s another treatment we can use for patients who are struggling with arthritis symptoms and want to avoid a TKA.”
| Barbara Boughton is a freelance writer based in the San Francisco Bay Area. |
Source Lower Extremity Review
| References |
- Gait using pneumatic brace for end-stage knee osteoarthritis, Kapadia BH, Cherian JJ, Starr R3, Chughtai M, Mont MA1, Harwin SF, Bhave A. J Knee Surg. 2016 Apr;29(3):218-23. doi: 10.1055/s-0036-1579790. Epub 2016 Mar 10.
- Osteoarthritis of the knee (non-arthroplasty), Evidence-based Guideline, 2nd edition. 2013. American Academy of Orthopaedic Surgeons. Published May 18, 2013.
- Strength and functional improvement using pneumatic brace with extension assist for end-stage knee osteoarthritis: A prospective randomized trial, Cherian JJ, Bhave A, Kapadia BH, Starr R, McElroy MJ, Mont MA. J Arthroplasty 2015;30(5):747-753.
- Clinical outcomes of a pneumatic unloader brace for Kellgren-Lawrence grades 3 to 4 osteoarthritis, Chughtai M, Bhave A, Khan SZ, Khlopas A, Ali O, Harwin SF, Mont MA. J Knee Surg. 2016 Nov;29(8):634-638. Epub 2016 Oct 17.
- Valgus bracing for knee osteoarthritis: A meta-analysis of randomized trials, Moyer RF, Birmingham TB, Bryant DM, Giffin JR, Marriott KA, Leitch KM. Arthritis Care Res (Hoboken). 2015 Apr;67(4):493-501. doi: 10.1002/acr.22472.
- The 2- and 8-week effects of decompressive brace use in people with medial compartment knee osteoarthritis, Lamberg EM, Streb R, Werner M, Kremenic I, Penna J. Prosthet Orthot Int. 2016 Aug;40(4):447-53. doi: 10.1177/0309364615589537. Epub 2015 Jun 25.
- Improvements in function and strength with decompressive bracing of the osteoarthritic knee, Lamberg, Eric M. EdD, PT; Streb, Robert PhD, PT; Werner, Marc CPO; Kremenic, Ian J. MEng; Penna, James MD. JPO Journal of Prosthetics & Orthotics: October 2016 – Volume 28 – Issue 4 – p 173–179 doi: 10.1097/JPO.0000000000000104
- Dynamic activity of unloader knee braces in genu varum subjects: New insights to improve compliance in medial knee osteoarthritis patients? Patrice Rougier, Etienne Cusin. Ann Phys Rehabil Med 2016;59S:e33. DOI: 10.1016/j.rehab.2016.07.078
- Immediate effect of valgus bracing on knee joint moments in meniscectomised patients: An exploratory study, Maria Thorning, Jonas B. Thorlund, Ewa M. Roos, Tim V. Wrigley, Michelle Hall. J Sci Med Sport 2016;19(12):964-969.
- Immediate effects of a brace on gait biomechanics for predominant lateral knee osteoarthritis and valgus misalignment after anterior cruciate ligament reconstruction, Hart HF, Collins NJ, Ackland DC, Cowan SM, Hunt MA, Crossley KM. Am J Sports Med. 2016 Apr;44(4):865-73. doi: 10.1177/0363546515624677. Epub 2016 Feb 3.
- Efficacy of unloader bracing in reducing symptoms of knee osteoarthritis, Ostrander RV, Leddon CE, Hackel JG, O’Grady CP, Roth CA.Am J Orthop (Belle Mead NJ). 2016 Jul-Aug;45(5):306-11.
| Further reading |
Braces and orthoses for treating osteoarthritis of the knee, Duivenvoorden T, Brouwer RW, van Raaij TM, Verhagen AP, Verhaar JA, Bierma-Zeinstra SM. Cochrane Database Syst Rev. 2015 Mar 16;(3):CD004020. doi: 10.1002/14651858.CD004020.pub3. Review. Full text